How Sick Are we as a Nation: The Health Crisis in the UK
- 12th Jul 2024
- Read time: 29 minutes
- Dr. Max Gowland
- Article
Today in the UK , there are around 68 million people, of whom nearly 20% are aged 65 and over.77 In fact, in the next decade, the number of over 65’s is expected to continue to rise further, driven by longer life expectations, better health and improved living conditions.
Certainly, the majority of individuals aspire to enjoy a lengthy and robust life, ideally extending well into their eighties and nineties, free from significant illnesses. Unfortunately, our current reality is far from this ideal, as statistics indicate that during the latter part of one's life, most people contend with some form of chronic health condition, and some experience frailty or disability prematurely. The prospect of merely enduring a long life is unappealing if it entails spending the last fifteen to twenty years grappling with a slew of chronic ailments or even disability. Instead of focusing solely on lifespan, we should shift our attention to health span as the new objective. Regrettably, this aspiration appears to be regressing rather than progressing.
1.1 OUR DECLINING HEALTH SPAN
Life expectancy has risen impressively over the last few decades, but more recently the curve has slowed, then flattened and the latest data actually shows a slight decline.1

Part of this decline will have been related to the COVID 19 pandemic of course, so more data will be needed over the coming years to ascertain if lifespan is genuinely falling. However, even the years prior to the epidemic, there is clear evidence of a slowing of the rate of life expectancy improvement, which is cause for concern.
What is far more worrying is the decline of healthy years lived without a disabling health condition.2

This graph, from recent Office for National Statistics (ONS) data, clearly shows how ‘healthy life expectancy’ has fallen dramatically for both men and women, with the fall in female health expectancy particularly worrying, as this shows that a women born in 2008 would on average live to 64 years old without a disabling health condition. This ONS data shows that on average, in 2020, females will now only have around 60 healthy years before the onset of a disabling chronic disease or some other disability. 2
In less than 15 years, women have lost nearly four years of healthy life.
The question to be asked is ‘what is driving this increase in sickness, the loss of health and also the loss of healthspan itself’?
With the discovery of penicillin in 1928 by Sir Alexander Fleming, the first antibiotic, Penicillin G became widely available across the world, kick starting the antibiotic revolution. Very quickly after the introduction of penicillin and other antibiotic wonder drugs, the leading causes of death moved from infectious diseases to chronic diseases. This was a huge breakthrough for medicine. 113
In established economies, the so called ‘communicable diseases’ now represent a small proportion of deaths and health issues, whereas the non-communicable diseases (NCDs) or ‘chronic diseases’ now represent around 80% of total disease burden, much of which can be avoided.3 A significant portion of this rise can be attributed to our aging demographic, which is more susceptible to chronic illnesses. Nonetheless, this cannot be solely attributed to age alone, or indeed genetics, but rather, lifestyle choices which can play a very significant role.
But let’s look firstly at the state of the UK’s health by visiting some numbers, which gives a snapshot picture of some relevant current health markers.

53% of the population reported that within the last fortnight, they had used medicines prescribed by their GP.
In a recent 2020 study carried out by the ONS, it was confirmed that 53% of the population reported that within the last fortnight, they had used medicines prescribed by their GP.4 This represents a substantial segment of the overall population reliant on medication and is undoubtedly a prominent indicator of our subpar health.
A more detailed snapshot of illnesses affecting people longer term, showed that 33% of people reported an allergy problem of one sort, 18% reported high blood pressure, over 20% were suffering spinal pain and 15% had depression. One other condition that is also worth mentioning is that 12% of people also reported having high blood lipids, which of course, is a precursor to cardiovascular disease and coronary heart diseases. 4 Of course, these are just the people who have received a diagnosis, so in reality, it is likely that the incidence of many of these disease states may be higher still.
Importantly, it is noteworthy that high blood pressure is a significant risk factor for stroke.196
1.2 CHRONIC DISEASE – A GROWING EPIDEMIC
A chronic disease is a long-lasting medical condition that typically progresses slowly and persists over a prolonged period, often for the rest of a person's life. These diseases are not contagious of course and are usually associated with complex, multifactorial causes. Examples of chronic diseases include heart disease, cardiovascular disease (CVD), type 2 diabetes (T2D), hypertension, non-alcoholic fatty liver disease (NAFLD), cancer, neurodegenerative disease, osteoporosis, sarcopenia, chronic obstructive pulmonary disease (COPD), musculo-skeletal problems and autoimmune disorders. 114
The rapid growth in the prevalence of chronic diseases is attributed to several interconnected risk factors. These include poor dietary choices, lack of exercise, obesity, high blood lipids and cholesterol, notably low density lipoprotein (LDL-C), air pollution, smoking, excessive alcohol consumption, excessive consumption of free sugars, sun exposure, genetics and of course increasing age itself. Even the lack of quality sleep on a regular basis has been shown to be associated with a range of chronic diseases including cardiovascular diseases and even cancers. 5, 6, 7
According to a study conducted by the UK's The Health Foundation’s REAL Centre, the duration individuals can anticipate living with a significant chronic illness is projected to rise from 11.2 years in 2019 to 12.6 years in 2040.
The prevalence of chronic diseases is expected to surge by over a third, affecting one in five individuals, primarily due to an aging population. The forecast below is notably alarming, revealing substantial increases in the prevalence of various diseases. For instance, diabetes is anticipated to increase by nearly 50%, and heart failure could nearly double. 97

Unfortunately, the trend continues in an upward trajectory, not only in the Western industrialised countries, but also across low- and middle-income countries, where rates of cardiovascular disease, diabetes and cancer have increased dramatically and are continuing to increase. A further trend is that of obesity, which again is increasing rapidly amongst low-income countries, which previously showed much low obesity levels. 3
Currently, the world sees around five births per second, and these newborns can expect longer lifespans, surpassing 69 years, which is about six years more than two decades ago. 3 Despite this, the overall well-being of these children is also under threat due to the rise of chronic diseases, now the leading cause of death globally, including in the United States. Over the last century, there has been a significant shift from communicable or infectious diseases being prevalent in non-industrialised countries, to chronic diseases burdening industrialised and modernised nations. This shift is ongoing, affecting heavily populated countries like China and Brazil. The surge in chronic diseases, as shown on the graphs below, has placed a substantial social, emotional, and economic strain on societies worldwide. 3

1.3 THE POWER OF EXERCISE
It is widely recognised and accepted that we should all stay active on a daily basis. The NHS for example encourages us to do some form of exercise every day.115 Their recommended exercise regime is around 150 minutes a week with a variety of strengthening activities, daily walks, and more vigorous aerobic exercise too, in order to get the heart pumping, raise the pulse and also get the lungs working hard. The key though, is to avoid sitting or lying down for extended periods of time, as it is well known that sedentary behaviour like this is a risk factor for a range of chronic diseases. Some say that ‘sitting is the new smoking’ highlighting the ill effects from being overly sedentary. Estimating the amount of time spent on exercise is always open to challenge, as the way in which we measure activity can be variable and open to interpretation. However, what is important is that the vast majority of people are simply not spending enough time moving, let alone exercising and this contributes to an unhealthy lifestyle.
Despite the NHS recommendation of exercising for at least 150 minutes per week, a recent YouGov publication alarmingly shows that over a third of UK adults fail to do any exercise at all, with only one in nine managing one exercise session per week.8

A recent YouGov paper alarmingly shows that over a third of UK adults fail to do any exercise at all.
Exercise has long been recognised as one of the most beneficial activities that can reduce risk of disease and its effects on health outcome. 116 In one Canadian study, the risk of mortality across a number of disease states, known as ‘all-cause mortality’, was reduced dramatically, in fact halved in some cases, demonstrating the significant and protective effects of regular exercise, as measured using METS (metabolic equivalents). This was observed across high blood pressure patients, those with COPD, type 2 diabetics and also those who smoked. People with high BMI or high total cholesterol (TC) also saw large risk reductions if they were exercising regularly. 66

In a recent 2021 paper from the National Library of Medicine, the authors cited studies in which people who engaged in even a relatively small amount of activity (>3,500 steps/day) reduced the risk of diabetes by as much as 30%. Higher volumes of exercise were also shown to reduce unhealthy fatty deposits within the liver, thereby lowering risk of non-alcoholic fatty liver disease (NAFLD). Other benefits included improved weight management, higher bone density and strength and even lower risk of various cancers too.67
For example, a recent 2019 systematic review concluded, after reviewing over 45 separate studies including some high-quality meta-analyses, that higher levels of physical activity were associated with lower levels of bladder, breast, colon, endometrial, oesophageal, adenocarcinoma, renal and gastric cancers. 76
There are countless scientific studies which repeatedly show the benefit of exercise on multiple health outcomes. 117 Some health professionals say that if exercise was available as a drug, then it would be the most powerful drug ever discovered in its ability to treat, or more importantly, help prevent many illnesses, especially chronic disease.
If exercise was available as a drug, then it would be the most powerful drug ever discovered to prevent disease.
1.4 THE GROWING OBESITY EPIDEMIC
It is well accepted that carrying excess weight is a risk factor for a wide range of quite serious chronic diseases. These include, cardiovascular disease, high blood pressure, type 2 diabetes, fatty liver disease and even a variety of cancers. 118
Over the last thirty years or so, more and more people find themselves in not only the overweight category (with a BMI of 25-30) but also within the obesity category (with a BMI of greater than 30). 9
Extracted from a recent National Food Strategy paper written by Henry Dimbleby, the three graphs below show how the weight of the population in the UK has quite rapidly grown over this time period, into what some call ‘the obesity epidemic’. 9, 99



It is quite extraordinary extraordinary how rapidly the obesity crisis has exploded, with no measurable presence of obesity in the 1950s. It is worth noting too, that a very small percentage of people were classified as only just overweight in the 1950s data.
A recent report from NHS Digital , shows that almost three quarters of adults, aged between 45-74 years old are living with overweight or obesity. The graph below shows that obesity, however, is not limited to middle aged adults either, with nearly 60% of 25-34 year olds also falling into the overweight/obese categories.10

What is especially worrying is that 10.1% of reception age children (aged 4-5 years) are also classed as obese, with a further 12.1% falling into the overweight category. In addition, those living in more deprived areas are even more likely to become overweight or obese, making these children much more prone to chronic disease and ill health, later on in their lives. 10
However, obesity statistics are just one of the initial indicators demonstrating that the population is becoming less healthy, experiencing a higher prevalence of illness, and increasingly susceptible to developing disabling chronic conditions at an earlier age. The biggest factor affecting our weight and our waistline of course, is our diet. Exercise will help control weight to some extent, but diet is by far the most significant contributor to a growing waistline and indeed our overall health too. 119
1.5 THE GROWING HEALTH RISKS OF TYPE 2 DIABETES

Both carbohydrates and fats contribute the majority of fuel for the body’s energy requirements. The carbohydrate source, comes mainly in the form of either complex carbohydrates, known as polysaccharides or sugar itself.
But too much sugar in the blood can become problematic. In fact, at any one time, we only have around five grams, or just a teaspoonful of glucose, within our entire vascular system. This means that control of sugar levels must be extremely precise and is generally controlled with two main hormones acting in synchrony. The first is insulin, which when released, causes glucose to become absorbed by the cells around the body and also stored as glycogen in both the muscle tissues and the liver, whilst glucagon, it’s opposite number, causes glucose to be released from the liver for immediate energy production, when glucose stores are low. 120
With type 2 diabetes, cells become less sensitive to the effects of insulin, making the pancreas produce even more. Over time, the pancreas can become stressed with the continuing demand to make increased levels of insulin, resulting in insulin levels which eventually cannot cope with the high sugar levels in the blood. These higher levels of glucose (hyperglycaemia) must be controlled, or this can lead to microvascular problems, retinopathy, kidney damage and atherosclerotic plaque build-up. In fact, each week, diabetes leads to nearly 200 amputations, 800 strokes, 600 heart attacks and over 2000 cases of heart failure. Diabetes is a serious chronic disease, and many are unaware of its grave consequences until it is too late. 11, 121
The latest headline from Diabetes UK, shows that 5 million people in the UK are already type 2 diabetic, when undiagnosed cases are included, with another 14 million believed to be pre-diabetic ie, just about to become diabetic if their blood sugar is not better controlled. 11 Type 2 diabetes is now another serious health epidemic, not only in the UK, but in all developed and even now, within developing economies. The annual cost to the NHS is a prohibitive £14 billion, caused mainly by the downstream health effects of type 2 diabetes and the ongoing and incessant treatment necessary, well into older age. 121, 11
Obesity is also a strong risk factor for acquiring diabetes and Diabetes UK are worried that the high numbers of people living with high BMI or obesity itself, is translating rapidly into type 2 diabetes. Chris Askew, the CEO of Diabetes UK said:
“These latest figures show we’re in the grip of a rapidly escalating diabetes crisis, with spiralling numbers of people now living with type 2 diabetes and millions at high risk of developing the condition. “ 11
Again, diet will play a key role here with both obesity and diabetes. But both these health indicators are getting worse and worse over time. Both the usual combination of both improved diet and also exercise, again will play the most powerful role in reversing or inhibiting the onset of both these chronic health problems over time. 202
1.6 CARDIOVASCULAR DISEASE CONTINUES TO BE THE LEADING CAUSE OF MORTALITY
Cardiovascular disease (CVD), a condition that can lead to both heart attacks and strokes, stands as the leading cause of death in the Western world. Specifically, in the UK, CVD is responsible for over a quarter of all deaths, accounting for approximately 170,000 fatalities annually. 12
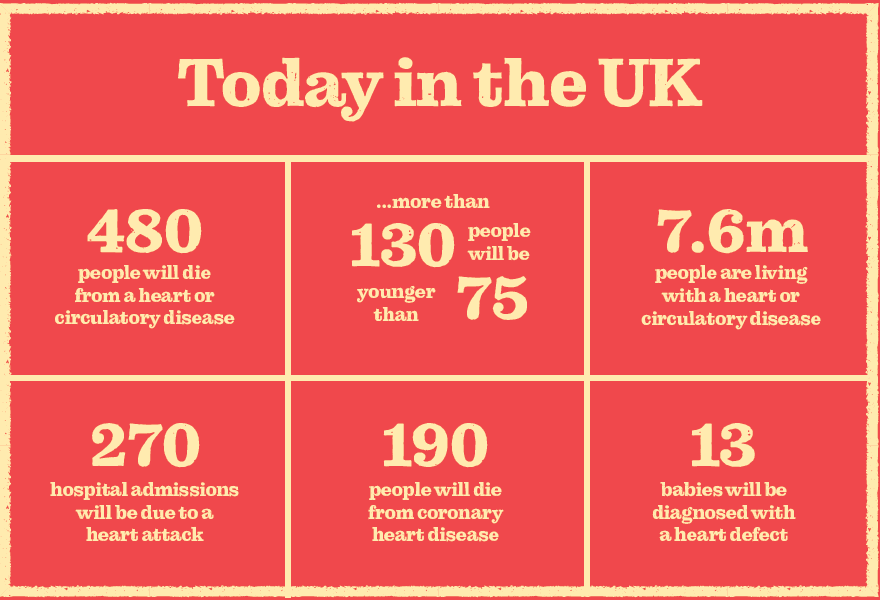
According to the UK’s British Heart Foundation (BHF), over 7 million people are today living with various forms of CVD, including coronary heart disease, atherosclerosis, atrial fibrillation, heart failure, stroke and also vascular dementia.12 Data taken from the BHF website show how CVD is translated into an alarmingly high level of daily, serious health incidents.
Seven out of ten people will survive a first heart attack, but this also means that for around 30% of people, their first heart attack is their last. 12
Cardiovascular disease is the leading cause of mortality in the Western World.
Risk factors associated with CVD include high blood lipids such as LDL cholesterol, high blood pressure, smoking, obesity, type 2 diabetes, poor sleep, stress and of course lack of physical activity, which plays an especially significant role. Age is also a non-modifiable risk factor. 12
But there is one particular risk factor which serves as a major precursor to a range of cardiovascular problems and that is atherosclerosis itself. Atherosclerotic cardiovascular disease (ASCVD) is the slow but incessant build-up of fatty plaques within the arteries. These plaques are typically the result of high levels of LDL cholesterol (LDL-C), otherwise known in the popular press as ‘bad’ cholesterol, and can actually start forming even in one’s teens, but do not cause any clinical problems until later in life, when the excessive fatty build up can start to cause arterial narrowing and blood flow problems and therefore increase the risk of a variety of cardiovascular diseases. Arterial stiffness can also be a consequence of ASCVD. 122
Incredibly, the heart beats around 100,000 times every day and pumps 5 litres of blood through nearly 60,000 miles of blood vessels. But the build-up of damaging atherosclerotic plaque will quickly put so much strain on this finely tuned cardiovascular system, that the heart and its vessels will decline in their health and their ability to perform their daily tasks. In addition, the blood vessels will become stiffer, raising blood pressure, and increasing the risk of stroke. 12
Cholesterol is known to play a key role in the onset of atherosclerosis and ultimately CVD. But cholesterol itself is a requirement of life with all our cells needing this key biochemical, most of which is made endogenously or within the body itself. Only a small fraction surprisingly, comes from food. But elevated levels of LDL cholesterol (low density lipoprotein) are strongly associated with CVD risk and some scientists believe actually plays a causal role in atherosclerotic plaque build-up. So, keeping LDL-C at bay is important if one is to lessen the risk of heart disease. 12
Though genetics to some minor extent, can play a role in ASCVD, 123 it is the quality of dietary intake that will more significantly influence the type and the degree of blood lipids present within the bloodstream.124 This is typically evaluated via a blood draw at the local GP surgery and can give a useful CVD risk factor based on the data from these blood tests, combined with a series of general lifestyle questions. Keeping LDL-C within acceptable limits is key to health, and diet will play a significant role in helping to achieve this target.
1.7 Non-Alcoholic Fatty Liver Disease-A Creeping Threat
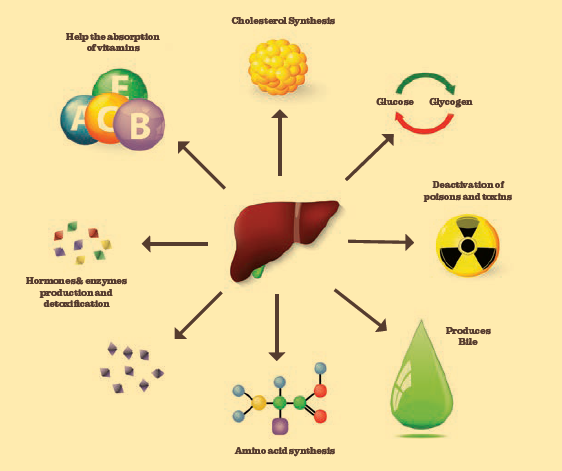
The liver is a truly incredible organ, weighing around 1.4 kilograms, situated in the upper quadrant of the abdominal cavity. It performs many thousands of complex chemical reactions and acts as the biochemical central processing unit of the body. The liver manages cholesterol, stores glucose for energy, rids the body of toxins, aids digestion and also makes hormones too. 125
However, the liver is prone to fatty deposits, especially if the diet is poor, with high saturated fat and over consumption of calories, especially ‘junk calories’ from ultra-processed foods. NAFLD is also common with people who have certain diseases and conditions, including obesity, type 2 diabetes. High blood lipids and also lack of physical activity. 127 Excessive fat in the liver cells is known as non-alcoholic fatty liver disease (NAFLD) which is now prevalent worldwide, and especially so in the developed economies. NAFLD is widely underappreciated as a leading chronic disease and is estimated to affect between 25-30% of the population. 126 If left untreated, NAFLD will undergo serious irreversible scarring or fibrosis. This more severe damage is referred to as non-alcoholic steatohepatitis (NASH). If not controlled or treated, this can lead to the more serious cirrhosis or end stage liver failure.14, 127

Non-alcoholic fatty liver disease affects over a quarter of the population.
NAFLD can be initially diagnosed via both blood test and ultrasound (Fibroscan) imaging techniques, looking at liver enzymes and liver stiffness respectively, with liver biopsy being the gold standard test as confirmation. It is worthy to also note that most pharmaceutical interventions fail to genuinely reverse the damage if it has progressed to the more serious next stage, known as non-alcoholic steatohepatitis (NASH), where initial fibrosis or scarring of the liver has commenced. 127
As with the other chronic diseases already mentioned, lifestyle modification such as improved diet and exercise, can again play a significant role in the inhibition of NAFLD and its reversibility, especially during early stages. Studies continue to demonstrate that poor quality diets are associated with NAFLD and that improvement in dietary patterns is an effective tool in the prevention of this underappreciated and serious chronic disease.
1.8 THE WIDESPREAD NATURE OF POOR MENTAL HEALTH AND STRESS
Mental health has unfortunately become a prevalent topic amongst media and social media discussions today. The latest data from the Office for National Statistics (ONS) indicates that approximately 12% of individuals self-report one or more periods of depression within a twelve-month timeframe. This statistic highlights the significant impact of mental health challenges on a significant percentage of the population.4

According to Priory, who is a leading independent provider of mental healthcare within the UK, nearly half of all adults claim that they have had a diagnosable mental health condition at some point in their lives. In fact, a fifth of men and a third of women have been diagnosed by a health professional for some form of a mental health condition. 53
Around 70% of people suffering from depression report a relatively mild form of the condition, but moderate to severe depression can also affect around 30% of cases. A deeper dive into the statistics shows that women are more likely to suffer from depression, affecting some 24%, compared to 13% of men.53
Depression is also responsible for the annual loss of 109 million working days each year in England alone, according to Priory, with a cost to the economy of around £9 billion. 53
Though related to mental health, stress is a phenomenon that arises as a response to a tricky situation. Stress is a perfectly natural response to these different situations, with some coping better than others. According to Priory, 79% of adults feel stressed at least one day each month, with 7% of people claiming that they feel stressed every single day. On an even more serious note, 32% of adults report that they have experienced suicidal feelings as a result of this stress. 53
Looking at anti-depressant medicines as another metric to measure the extent of the problem, according to the uk.gov website, around 17 % of people were taking a drug, typically SSRIs (serotonin selective reuptake inhibitors), in order to help manage their depression. These work by increasing serotonin levels in the brain.17 In fact in 2021, over 20 million anti-depressant drugs were prescribed in the UK, representing a 3% increase compared to the previous year.18
Depression is an increasingly prevalent and genuine concern, presenting itself across a broad spectrum of disorders. When left unmanaged, it can escalate rapidly, leading to significantly graver outcomes. 32 Any discussion about the nation's health must include this crucial health domain. As explored in the following section of this paper, the 'SMILES trial' conducted in 2015 provides substantial evidence demonstrating the impact of diet quality on the mental well-being of individuals. 92
1.9 THE IMPORTANCE OF OVERALL METABOLIC HEALTH
"Metabolic health" refers to the overall state and functionality of an individual's metabolism. It encompasses how efficiently the body processes and utilises energy from the foods we consume, manages blood sugar levels, controls cholesterol, regulates blood pressure, and handles many other aspects of metabolism. 128
A person is considered metabolically healthy when their metabolic processes are functioning optimally, resulting in balanced blood sugar levels, healthy cholesterol levels, appropriate blood pressure, and a well-managed body weight. In contrast, metabolic dysfunction or poor metabolic health can manifest as insulin resistance, obesity, diabetes, high blood pressure, and abnormal lipid profiles. 128
Maintaining good metabolic health is crucial for overall well-being and can significantly impact an individual's risk for a variety of chronic diseases, including type 2 diabetes, cardiovascular diseases, non-alcoholic fatty liver disease and other metabolic disorders. Lifestyle factors such as a balanced diet, regular physical activity, adequate sleep, and stress management play pivotal roles in promoting and sustaining metabolic health. Additionally, monitoring and managing key indicators of metabolic health through regular health check-ups and screenings are essential for preventive healthcare. In more detail, some of the risk factors for poor metabolic health are listed below: 128
Cardiovascular Health: A healthy metabolism helps regulate factors like blood pressure, LDL cholesterol levels, and general systemic inflammation, which are closely linked to overall cardiovascular health. Imbalances in metabolism can contribute to the development of a range of cardiovascular diseases. 129
Type 2 Diabetes: Metabolism plays a key role in managing blood sugar levels. Insulin resistance, a hallmark of type 2 diabetes, disrupts the body's ability to regulate glucose effectively, which can lead to a cascade of related health problems, as described previously. 129
NAFLD (Non-Alcoholic Fatty Liver Disease): Metabolic issues can also lead to the accumulation of unwanted visceral fat in the liver, resulting in NAFLD. This condition is linked to insulin resistance and other metabolic disturbances and can lead on to much more serious health issues concerning the liver, if not managed. 129
High Blood Pressure: Disruptions in metabolism can contribute to imbalances in hormones and biochemicals that regulate blood vessel constriction and dilation, affecting blood pressure regulation. A poor diet too can lead to high blood pressure. High blood pressure is a risk factor for stroke. 129
High Blood Sugar: High blood sugar levels, often associated with diabetes, can result from metabolic dysfunction that impairs the body's ability to properly utilise and regulate blood glucose. Glucose regulation must be finely tuned and any alteration in glucose levels will have a range of negative downstream health issues, in addition to diabetes itself. 129
High Levels of LDL Cholesterol: Metabolic imbalances can lead to higher levels of low-density lipoprotein cholesterol (LDL-C), often referred to as "bad" cholesterol, which is a risk factor for cardiovascular disease and the build-up of atherosclerotic fatty plaques. 129
Obesity: Metabolic health and obesity are very closely linked. Obesity can lead to insulin resistance and general inflammation, contributing to the development of various metabolic disorders. 129
It's important to note that these risk factors and conditions are often very much interconnected. For example, obesity can contribute to insulin resistance, which in turn increases the risk of type 2 diabetes and other metabolic disorders. Similarly, poor metabolic health can exacerbate multiple cardiovascular issues.
Metabolic Syndrome
Our overall metabolic health determines both our lifespan and also our health span too. In fact, scientists have grouped a number of these risk factors into a condition known as ‘metabolic syndrome’, also known as syndrome X. This cluster typically includes abdominal obesity and excessive waistline, high blood pressure, insulin resistance and high blood sugar, high triglyceride fats and a low level of HDL cholesterol (HDL-C), known as the ‘good cholesterol’. If just three of these risk factors are present, then the person is deemed to have metabolic syndrome and will be prone to a series of chronic diseases including cardiovascular disease, type 2 diabetes, fatty liver, gallstones, and even some forms of cancer. 15 Data from the National Heart, Lung and Blood Institute in the USA have calculated that around one in three Americans and around one in four in the UK are currently suffering from metabolic syndrome and this health indicator is also increasing over time. 73, 130
About a quarter to one third of adults are suffering from metabolic syndrome.
Our overall metabolic health is so dependent on the quality and the balance of our diet and is also influenced greatly by how active we are and the frequency of exercise. 131
We have mentioned the importance of exercise multiple times but have not yet considered how healthy our diet is compared to where it should be. Over the years, various health messages and dietary targets have been established by policymakers, yet the majority of individuals seem to have either disregarded them or not taken them seriously. These include messaging such as the ‘five a day’, or ‘low fat’ guidelines or even the more recent ‘alcohol is a carcinogen’ television advertisements, none of which seem to have made any meaningly impact on our diets. Sadly, these healthy eating initiatives seem to have failed and still are seen as confusing to many consumers, the reasons of which will not be covered in this position paper. 132, 133
1.10 HOW POOR MUSCULO-SKELETAL HEALTH CAN LEAD TO EARLY FRAILTY
An overview on health must also include the topic of musculoskeletal health. This refers to a combination of overall muscle strength and muscle mass, bone density, general joint health and overall flexibility. This group of health areas is what allows us to perform daily activities effectively with no second thought.

However, staying active is a crucial factor in the maintenance of our musculoskeletal health. 134 The popular saying ‘use it or lose it’ holds true in scientific terms, as research confirms that muscle loss occurs when muscles are disused, especially after middle age and this loss of muscle continues to accelerate even faster as one ages further. This is known as ‘sarcopenia’. This early loss of muscle strength can accelerate an individual’s trajectory to what is called the ‘disability threshold’ , as cited in the graphic, where they can become frail and can no longer perform routine daily activities independently. 135
Bone strength too is another important requirement if one is to avoid fractures. A lack of weight bearing exercise can be a recipe for weak bone structure and bone density, thereby raising fracture risk. As with muscle loss, this will worsen with age, with menopausal women especially, losing quite significant bone density and bone strength, raising fracture risk considerably. 16
Data from musculo-skeletal research shows that a hip fracture after the age of 65 years can be profoundly serious, with around a quarter of people dying within the first twelve months following surgery, a truly frightening statistic.78 Protecting bone strength is clearly of paramount importance.
Maximum bone density occurs at around 30-35 years old and then it is a matter of protecting this bone strength with weight bearing exercise, combined with plenty of vitamin D and enough calcium too. Both these nutrients tend to be low in most people’s diets according to diet and nutrition surveys, making supplementation a sensible option to many, especially older adults. 136
Another critical aspect within the domain of musculoskeletal health is joint health with 8 million people in the UK currently living with this condition. 137 . Issues in this area can pose significant challenges, resulting in substantial costs to the healthcare system, estimated to be approximately £10 billion per annum. Furthermore, this can lead to huge losses in productivity, estimated to be around a loss of over 30 million working days, around 22% of toral sickness absence.137 An optimal, healthy joint comprises bones separated by a collagen-rich cartilaginous layer. This, combined with a lubricating synovial fluid, enables smooth joint movement without pain or stiffness.
However, joint tissues are susceptible to various forms of damage, including injuries, overuse, and constant exposure to energetic and pro-inflammatory free radical attack. These factors can lead to the deterioration of the joint, causing chronic degeneration and inflammation. 138 The World Health Organisation (WHO) recognises this chronic degeneration and inflammation of the joint, as one of the most disabling conditions in developed countries. 139
Maintaining a healthy, well-balanced diet along with regular exercise remains a widely recognised and effective approach for ensuring long lasting and trouble-free joints. However, current data suggests that a significant portion of the population falls short of meeting the recommended levels of physical activity.
Insufficient physical activity can lead to inflamed, stiff, and painful joints. Arthritis UK reports that approximately 10 million people in the UK are presently dealing with osteoarthritis (OA), a condition that can affect individuals across various age groups, not just older adults. Obesity is a notable risk factor for OA due to the additional pressure it places on joint mechanics. 140
A person experiencing stiffness and pain in their joints may find movement and exercise uncomfortable, leading them to adopt a more sedentary lifestyle. Unfortunately, this increased sedentary behaviour can exacerbate the loss of muscle strength and further deteriorate joint health, perpetuating a detrimental 'vicious cycle' towards frailty and overall poor health. Therefore, emphasising and prioritising one's musculoskeletal health is crucial.
Breaking this cycle is quite possible through a combination of a healthy diet and regular exercise. However, regrettably, a considerable number of people still struggle to maintain both a nutritious diet and a consistent exercise routine, underlining the urgent need for education and support in promoting these essential lifestyle changes. 140
1.11 SUMMARY
-
In the UK, dietary factors were responsible for 17% of all deaths, indicating a critical health concern.
-
Lifespan has now plateaued, with actual number of healthy years or healthspan, reported to be declining over the past two decades, with women in particular experiencing nearly a four-year reduction in healthy life.
-
Approximately 53% of the population are having to use prescription medication, as reported within the last two weeks.
-
Chronic diseases are on the rise in the Western world, including a growing obesity epidemic where almost three-quarters of those over 45 are either overweight or obese.
-
Obesity is linked to and fuelling various chronic diseases, such as cardiovascular disease, type 2 diabetes and non-alcoholic fatty liver disease, affecting millions of individuals.
-
There are now 5 million people in the UK with diagnosed type 2 diabetes with another 13 million who are judged to be pre-diabetic.
-
Cardiovascular disease stands as the leading cause of death in the Western world, often related to high LDL cholesterol levels and fatty plaques.
-
Non-alcoholic fatty liver disease affects around a quarter of the population with much greater levels of this disease seen in obese patients. If left unchecked, this can lead to much more serious liver damage.
-
Musculoskeletal health and loss of general strength, mobility and balance will contribute to a sedentary lifestyle, increasing the risk of many chronic diseases.
-
Mental health issues, including depression and stress, affect significant numbers of the population, impacting well-being, health and productivity.
-
Metabolic syndrome, an unhealthy state, affects about one-third of adults and is associated with a range of inter-connected chronic diseases.


